Eyedrop Guide: A Comprehensive Overview (Updated 01/26/2026)
This guide details various eyedrop types – artificial tears, antihistamines, antibiotics, glaucoma, and steroids – addressing dryness, allergies, infections, and inflammation effectively․
Eyedrops are topical medications designed for the eye, delivering medication directly to the ocular surface․ They represent a cornerstone in managing a diverse range of eye conditions, from common dryness and allergies to more serious infections and chronic diseases like glaucoma․ Understanding the different types available, their specific functions, and proper administration techniques is crucial for effective treatment and maintaining optimal eye health․
The world of eyedrops encompasses a broad spectrum of formulations, each tailored to address specific needs․ These solutions aren’t merely for discomfort; they actively combat disease and preserve vision․ Choosing the right eyedrop, whether over-the-counter or prescription, requires informed decision-making, often in consultation with an eye care professional․
Why Use Eyedrops? Common Eye Conditions
Eyedrops are frequently used to alleviate discomfort and treat a wide array of common eye conditions․ Dry eye, a prevalent issue, benefits significantly from artificial tears, providing lubrication and relief․ Allergies trigger inflammation and itching, effectively managed with antihistamine eyedrops․ Bacterial conjunctivitis, or pinkeye, necessitates antibiotic eyedrops to combat infection․
More serious conditions, like glaucoma, require specialized drops to lower intraocular pressure, preventing optic nerve damage․ Even simple redness and irritation can be temporarily soothed, though reliance on redness-relieving drops should be cautious due to potential tolerance․ Addressing these conditions promptly with appropriate eyedrops is vital for preserving vision and quality of life․
Types of Eyedrops: A Detailed Breakdown
The world of eyedrops encompasses a diverse range of formulations designed for specific needs․ Artificial tears offer basic hydration, while antihistamine drops target allergic reactions, reducing itchiness and redness․ Antibiotic eyedrops are crucial for fighting bacterial infections, requiring a doctor’s prescription․ Glaucoma eyedrops manage intraocular pressure, preventing vision loss, and necessitate ongoing medical supervision․

Steroid eyedrops powerfully reduce inflammation but carry potential side effects, demanding careful use under a physician’s guidance․ Nighttime formulations provide enhanced hydration during sleep, and redness-relieving drops offer temporary cosmetic relief․ Understanding these distinctions is key to selecting the appropriate treatment․
Artificial Tears: For Dryness and Comfort
Artificial tears are the cornerstone of dry eye management, providing lubrication and relieving discomfort․ These drops mimic natural tears, supplementing insufficient tear production or improving tear quality․ Available over-the-counter, they come in various viscosities, from watery solutions for mild dryness to thicker gels for more severe cases․
Some contain preservatives, which can cause irritation with frequent use; preservative-free options are ideal for sensitive eyes or those needing frequent application․ While generally safe, occasional blurry vision can occur temporarily․ They are a first-line treatment, offering immediate, soothing relief from dryness, irritation, and a gritty sensation․
Antihistamine Eyedrops: Allergy Relief
Antihistamine eyedrops are specifically formulated to combat allergic conjunctivitis, relieving itchy, watery, and red eyes caused by allergens like pollen, dust, or pet dander․ These drops work by blocking histamine, a chemical released during an allergic reaction․ They provide rapid relief from allergy symptoms, often within minutes of application․
Available both over-the-counter and by prescription, some formulations also contain mast cell stabilizers for longer-lasting effects․ Common side effects include temporary stinging or burning․ Consistent use during allergy season can prevent symptoms, offering sustained comfort․ They are a targeted solution for allergy-related eye discomfort․
Antibiotic Eyedrops: Fighting Infections
Antibiotic eyedrops are crucial for treating bacterial eye infections, such as conjunctivitis (pinkeye) and corneal ulcers․ These drops directly target and eliminate the bacteria causing the infection, reducing inflammation and promoting healing․ They are typically prescribed by a doctor after a proper diagnosis, as not all eye conditions require antibiotics․
It’s vital to complete the full course of treatment, even if symptoms improve, to prevent antibiotic resistance and ensure the infection is fully eradicated․ Potential side effects include temporary stinging, burning, or blurred vision․ Prompt treatment with antibiotic eyedrops can prevent serious complications․
Glaucoma Eyedrops: Managing Intraocular Pressure
Glaucoma eyedrops are primarily used to lower intraocular pressure (IOP), the fluid pressure inside the eye, which is a major risk factor for glaucoma․ Different types of drops work in various ways – some decrease fluid production, while others increase fluid outflow․ Consistent use, as prescribed by an ophthalmologist, is essential to prevent optic nerve damage and vision loss․
Common side effects can include stinging, burning, blurred vision, and changes in iris color․ Regular monitoring by an eye doctor is crucial to assess effectiveness and manage any adverse reactions․ These drops help slow disease progression, preserving sight for longer․
Steroid Eyedrops: Reducing Inflammation
Steroid eyedrops are potent medications used to quickly reduce inflammation associated with various eye conditions, such as uveitis, severe allergic reactions, and post-surgical inflammation․ They work by suppressing the immune response in the eye, alleviating redness, swelling, and pain․ However, due to their strength, they are typically prescribed for short-term use only․
Long-term use can lead to serious side effects, including increased risk of cataracts and glaucoma․ Careful monitoring by an ophthalmologist is vital to manage potential complications and ensure appropriate dosage․ These drops require a prescription and should never be self-administered․
Understanding Eyedrop Ingredients
Eyedrops contain two primary components: active ingredients, which provide the therapeutic effect, and inactive ingredients, including preservatives and vehicles․ Common active ingredients target specific conditions – antihistamines for allergies, antibiotics for infections, and steroids for inflammation․ Preservatives, like benzalkonium chloride, prevent contamination after opening, but can sometimes cause irritation or allergic reactions in sensitive individuals․
Understanding these ingredients is crucial․ Some formulations are preservative-free, ideal for frequent use․ The vehicle delivers the active ingredient; it’s often purified water․ Always review the ingredient list and discuss any concerns with your doctor or pharmacist․
Common Preservatives in Eyedrops
Preservatives in eyedrops are vital for maintaining sterility after the bottle is opened, preventing bacterial contamination․ Benzalkonium chloride (BAK) is a frequently used preservative, effective against a broad spectrum of microbes․ However, BAK can sometimes cause ocular surface irritation, dryness, and even allergic reactions in susceptible individuals with prolonged use․

Other preservatives include polyquaternium-1 and stabilized oxychloro complex․ Preservative-free options are available, particularly recommended for those needing frequent applications or with sensitive eyes․ While more expensive, they minimize potential adverse reactions and are gentler on the ocular surface․
Active Ingredients and Their Functions
Active ingredients dictate an eyedrop’s purpose․ Artificial tears utilize polymers like carboxymethylcellulose or polyethylene glycol to lubricate and hydrate the eyes, relieving dryness․ Antihistamine drops contain medications like ketotifen to block histamine, easing allergy symptoms like itching and redness․
Antibiotic eyedrops feature antibiotics such as polymyxin B or tobramycin to combat bacterial infections․ Glaucoma drops employ various compounds—prostaglandins, beta-blockers, or carbonic anhydrase inhibitors—to lower intraocular pressure․ Steroid drops contain corticosteroids to reduce inflammation, but long-term use requires careful monitoring․
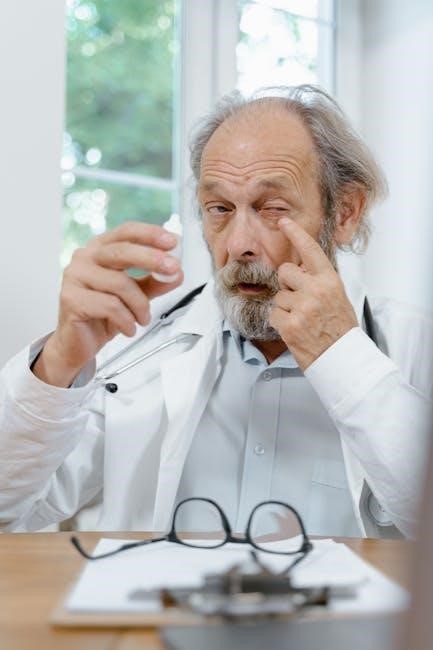
How to Properly Administer Eyedrops
Proper technique ensures effectiveness and minimizes contamination․ Begin by washing your hands thoroughly․ Gently tilt your head back and pull down your lower eyelid to create a pouch․ Hold the eyedrop bottle close to your eye, avoiding contact with the eye or surrounding tissues․
Instill one drop into the pouch, then gently close your eyes for 1-2 minutes․ Avoid blinking excessively, which can reduce absorption․ To prevent contamination, never touch the dropper tip to any surface․ Replace the cap securely after each use, and discard the bottle after the expiration date․

Preparing to Apply Eyedrops
Before administering eyedrops, meticulous preparation is crucial for optimal results and hygiene․ Begin by thoroughly washing your hands with soap and warm water, ensuring all traces of dirt or lotion are removed․ Gently remove any contact lenses you may be wearing, as they can interfere with medication absorption and potentially cause irritation․
Tilt your head slightly backward and gaze upwards․ Use a clean tissue or your fingers to gently pull down your lower eyelid, creating a small pocket to receive the drop․ This positioning helps prevent the drop from missing your eye and ensures better contact time․
The Correct Technique for Instillation
Hold the eyedrop bottle firmly, keeping the tip pointed downwards, but avoiding any contact with your eye or surrounding tissues․ Gently squeeze the bottle to release a single drop into the created pocket within your lower eyelid․ Avoid blinking immediately after instillation; keep your eye open for approximately 30 seconds to allow the medication to spread effectively across the surface․
After 30 seconds, gently close your eyes and apply slight pressure to the inner corner of your eye, near your nose․ This helps to prevent the medication from draining into your tear duct and ensures better absorption․ Repeat the process for the other eye, if prescribed․

Avoiding Contamination of Eyedrop Bottles
To prevent introducing bacteria and maintain sterility, never allow the tip of the eyedrop bottle to touch any surface, including your eye, fingers, or clothing․ After each use, securely replace the cap, ensuring it’s tightly closed․ Avoid sharing your eyedrops with others, even if they exhibit similar symptoms, as this can spread infection․
Store the bottle in a clean, dry place, away from direct sunlight and extreme temperatures․ If you suspect contamination – such as a change in color or cloudiness – discard the bottle and obtain a new one․ Proper handling safeguards your eye health․
Potential Side Effects of Eyedrops
While generally safe, eyedrops can cause temporary discomfort like stinging, burning, or blurred vision immediately after application; these usually subside quickly․ Redness-relieving drops may lead to dilated pupils and rebound redness with prolonged use, creating tolerance․ Less common, but serious, side effects require immediate medical attention․
Artificial tears can sometimes cause temporary cloudy vision․ Be vigilant for any unusual or persistent symptoms, such as increased pain, vision changes, or allergic reactions․ Always consult a healthcare professional if you experience concerning side effects after using any eyedrop formulation․
Common Side Effects: Stinging, Burning, Blurred Vision
Immediately following eyedrop administration, a transient stinging or burning sensation is frequently reported, representing a normal reaction as the liquid contacts the corneal surface․ Temporary blurred vision is also common, typically resolving within a minute or two as the drop disperses and vision adjusts․ These effects are generally mild and don’t necessitate discontinuing use․
However, if stinging or burning is severe or persists, or if blurred vision is prolonged, consult your eye care provider․ These symptoms could indicate an adverse reaction or underlying issue․ Most individuals tolerate these minor side effects without significant issue․
Less Common, More Serious Side Effects
While infrequent, serious side effects from eyedrops require immediate medical attention․ These can include severe eye pain, significant vision changes (beyond temporary blurring), swelling of the eyelids, or increased light sensitivity․ Allergic reactions manifesting as itching, rash, or difficulty breathing are also concerning․
Redness-relieving drops, used frequently, can lead to rebound congestion – worsening redness upon discontinuation․ Prolonged steroid use carries risks like glaucoma or cataracts․ If you experience any unusual or concerning symptoms after using eyedrops, discontinue use and consult an ophthalmologist promptly for diagnosis and treatment․
Developing Tolerance to Redness-Relieving Drops
Frequent use of redness-relieving eyedrops can unfortunately lead to tolerance, diminishing their effectiveness over time․ These drops primarily constrict blood vessels, temporarily whitening the eye․ However, with continued use, the eyes can become reliant on this constriction, resulting in “rebound redness” – where the redness worsens when the drops are stopped․
This cycle encourages increased drop usage, exacerbating the problem․ To avoid this, limit redness-relieving drop use and address the underlying cause of redness, such as dryness or allergies․ Consider artificial tears for lubrication or consult an eye doctor for a proper diagnosis and long-term solution․
Over-the-Counter (OTC) vs․ Prescription Eyedrops
Over-the-counter (OTC) eyedrops, like artificial tears and some antihistamines, are readily available for common, minor irritations such as dryness, redness, and mild allergies․ They offer temporary relief and are suitable for self-treatment of uncomplicated symptoms․ However, if symptoms persist or worsen, or if you suspect an infection or more serious condition, a prescription is necessary․
Prescription eyedrops address more complex issues like glaucoma, bacterial infections, and severe inflammation․ These require a doctor’s evaluation to diagnose the condition accurately and prescribe the appropriate medication and dosage․ Self-treating serious eye problems can lead to vision loss, so professional guidance is crucial․
When to Choose OTC Eyedrops
Opt for over-the-counter (OTC) eyedrops when experiencing minor, temporary eye discomfort; These are ideal for alleviating symptoms like dryness caused by environmental factors, extended screen time, or mild irritation․ Redness-relieving drops can provide quick, though temporary, relief from minor eye redness․ Antihistamine OTC drops are suitable for seasonal allergy symptoms like itching and watering․
However, remember OTC drops offer symptomatic relief, not a cure․ If discomfort persists beyond a few days, intensifies, or is accompanied by pain, vision changes, or discharge, discontinue use and consult an eye care professional․ OTC options are best for self-limiting conditions․
When a Prescription is Necessary
A prescription is crucial when dealing with eye conditions requiring specific medical intervention․ This includes bacterial or viral eye infections needing antibiotic eyedrops, and conditions like glaucoma demanding pressure-reducing medications․ If OTC remedies fail or your eyes stop responding, a professional evaluation is vital․
Severe allergies causing significant discomfort also warrant a prescription․ Furthermore, any sudden changes in vision, eye pain, or noticeable eye damage necessitate immediate medical attention․ Prescription eyedrops offer targeted treatment and monitoring, ensuring appropriate management of underlying eye health issues beyond the scope of self-treatment․
Eyedrop Storage and Shelf Life
Proper storage is paramount for maintaining eyedrop sterility and effectiveness․ Keep bottles in a cool, dry place, away from direct sunlight and extreme temperatures․ Avoid storing them in the bathroom due to humidity․ Always tightly close the cap after each use to prevent contamination․
Pay close attention to expiration dates printed on the packaging; using expired drops can be ineffective or even harmful․ Discard drops after the expiration date or within a specified timeframe post-opening – typically 28-90 days, depending on the formulation․ Regularly inspect for discoloration or cloudiness, indicating spoilage, and discard immediately if observed․
Proper Storage Conditions
Maintaining optimal storage conditions is crucial for preserving the sterility and potency of your eyedrops․ Ideally, store them in a cool, dry environment, shielded from direct sunlight and fluctuating temperatures․ Avoid locations prone to humidity, such as the bathroom, as moisture can compromise the solution․
Ensure the bottle cap is securely tightened after each use to prevent contamination from bacteria or other environmental factors․ Do not refrigerate unless specifically instructed by your doctor or the product label, as cold temperatures can alter the formulation․ Consistent, proper storage extends the shelf life and ensures the drops remain safe and effective․
Determining Expiration Dates
Always check the expiration date printed on the eyedrop bottle or packaging before each use․ Expired eyedrops may lose their effectiveness or, more seriously, become contaminated with bacteria, potentially causing an eye infection․ Discard any drops past their expiration date, even if they appear visually normal․
If the bottle doesn’t have a clearly visible expiration date, a general rule is to discard them within 28 days of opening․ Note the date you first opened the bottle to track this timeframe․ Pay attention to any changes in color, clarity, or odor, as these can also indicate spoilage, regardless of the expiration date․

Interactions Between Eyedrops and Other Medications
Eyedrops, even over-the-counter varieties, can potentially interact with other medications you’re taking, both oral and topical․ Certain ingredients might amplify or diminish the effects of other drugs, leading to unintended consequences․ For example, glaucoma drops could interact with heart medications․
It’s crucial to inform your doctor and pharmacist about all medications you use, including eyedrops, vitamins, and herbal supplements․ This allows them to assess potential interactions and adjust your treatment plan accordingly; Never assume an interaction isn’t possible; proactive communication is key to safe medication management․
Potential Drug Interactions
Several drug interactions can occur with various eyedrop formulations․ Glaucoma medications, for instance, may interact with beta-blockers or calcium channel blockers, potentially exacerbating cardiovascular effects․ Redness-relieving drops containing vasoconstrictors could interact with certain antidepressants or blood pressure medications․
Systemic absorption of eyedrop ingredients is possible, even with topical application․ This means the drug can enter the bloodstream and affect other organs․ Always disclose your complete medication list to your healthcare provider to avoid potentially harmful combinations and ensure your safety․ Careful monitoring is essential․
Informing Your Doctor About All Medications
Comprehensive disclosure of all medications is crucial when using eyedrops․ This includes prescription drugs, over-the-counter medications, herbal supplements, and vitamins․ Even seemingly unrelated medications can interact with eyedrop components, altering their effectiveness or increasing the risk of adverse effects․

Specifically, inform your doctor about any cardiovascular medications, antidepressants, or other drugs affecting blood pressure․ Accurate information allows for a thorough assessment of potential interactions, ensuring safe and effective treatment․ Don’t hesitate to ask your doctor about potential risks and necessary precautions․
Specific Eyedrop Formulations
Beyond standard types, specialized formulations cater to unique needs․ Nighttime dry eye drops, for instance, utilize thicker, longer-lasting lubricants to provide enhanced hydration during sleep, combating overnight dryness and morning discomfort․ Redness-relieving eyedrops offer temporary relief from minor irritation, utilizing vasoconstrictors to reduce visible redness․
However, prolonged use of redness-relieving drops can lead to tolerance and rebound congestion․ Understanding the specific purpose and limitations of each formulation is vital for optimal eye health․ Always consult with an eye care professional to determine the most appropriate option for your individual condition․
Nighttime Dry Eye Drops: Enhanced Hydration
Nighttime dry eye drops are specifically formulated to provide extended relief from dryness while you sleep․ Unlike regular artificial tears, these often feature thicker viscosities and oil-based components, creating a longer-lasting protective barrier on the ocular surface․ This minimizes evaporation and prevents discomfort during crucial overnight restorative processes․
They are designed to reduce morning grittiness and irritation, addressing dryness that accumulates during sleep when blinking is reduced․ These drops are generally preservative-free to minimize irritation, and their enhanced hydration supports overall corneal health․ Consistent use can significantly improve daytime comfort․
Redness-Relieving Eyedrops: Temporary Relief
Redness-relieving eyedrops offer quick, though temporary, relief from minor eye irritation and redness․ These drops typically contain vasoconstrictors, which constrict blood vessels in the conjunctiva, reducing visible redness․ However, it’s crucial to understand they don’t address the underlying cause of the irritation, only the symptom․
Prolonged or frequent use can lead to rebound redness – where the eyes become even redder when the drops wear off – and potential tolerance․ Side effects can include burning, stinging, and dilated pupils․ They are best used sparingly for occasional relief, not as a long-term solution for chronic eye issues․
Troubleshooting Common Eyedrop Issues
If eyedrops aren’t working, ensure you’re using the correct type for your condition and that the medication hasn’t expired․ Discomfort after application, like stinging or burning, is usually temporary, but persistent pain warrants a doctor’s visit; Check for allergies to ingredients․
If drops consistently fail to improve symptoms, or you notice any troubling side effects, discontinue use and consult an eye care professional․ Sometimes, the issue isn’t the drops themselves, but an underlying condition requiring different treatment․ Don’t self-treat prolonged or severe eye problems․
Eyedrops Not Working Effectively
Several factors can contribute to ineffective eyedrops․ First, verify you’re using the correct type for your specific eye issue – artificial tears won’t treat an infection․ Ensure the drops haven’t expired, as potency diminishes over time․ Proper instillation is crucial; a missed eye or improper technique reduces effectiveness․
Consider if other medications or underlying health conditions might interfere with absorption or efficacy․ If problems persist, consult your doctor․ They can reassess your diagnosis, adjust your treatment plan, or explore alternative formulations for better results․ Don’t continue using ineffective drops without professional guidance․

Dealing with Discomfort After Application
Mild stinging or burning immediately after applying eyedrops is common and usually subsides quickly․ Blurring vision is also typical, lasting less than a minute․ If discomfort persists or intensifies, gently blink several times to distribute the drops․ Avoid rubbing your eyes, as this can worsen irritation․
For prolonged discomfort, ensure you’re not allergic to any ingredients․ If redness, swelling, or pain develops, discontinue use and consult a doctor․ Some redness-relieving drops can cause rebound redness with continued use, requiring a break from the product․ Cool compresses can offer temporary relief․
The Future of Eyedrop Technology
The future of eyedrop technology focuses on innovative drug delivery systems, moving beyond traditional formulations․ Researchers are exploring nanoparticles and micro-inserts for sustained release, reducing the need for frequent application and improving efficacy; Personalized eyedrop formulations, tailored to an individual’s specific eye condition and tear film composition, are also on the horizon․
These advancements aim to enhance patient compliance and minimize side effects․ Smart eyedrops, potentially incorporating sensors, could monitor intraocular pressure or inflammation levels, providing real-time data for optimized treatment․ This represents a significant leap towards proactive and precision eye care․
Novel Drug Delivery Systems
Current research intensely explores novel drug delivery systems to revolutionize how medications reach the eye․ Nanoparticles offer targeted delivery, enhancing drug penetration and reducing systemic side effects․ Micro-inserts, tiny devices placed in the eye, provide sustained release over weeks or months, eliminating the need for daily drops․
These systems aim to overcome challenges like rapid tear turnover and poor corneal permeability․ Further development includes stimuli-responsive formulations, releasing medication based on specific eye conditions․ These innovative approaches promise improved treatment outcomes and patient convenience, marking a significant advancement in ophthalmic care․
Personalized Eyedrop Formulations
The future of eyedrop therapy leans towards personalized formulations, tailored to individual patient needs․ Genetic predispositions, tear film characteristics, and specific disease biomarkers will guide customized medication selection and concentration․ Diagnostic tools will analyze individual eye physiology, enabling precise treatment plans․
This approach moves beyond “one-size-fits-all” solutions, maximizing efficacy and minimizing adverse reactions․ 3D printing technology could create bespoke drops, combining multiple active ingredients in specific ratios․ Ultimately, personalized eyedrops represent a paradigm shift, optimizing ocular health outcomes for each patient․
